Advertisement
BMC Pregnancy and Childbirth volume 24, Article number: 805 (2024)
Metrics details
The issue of whether abortion increases the risk of future mental health problems for women remains a debated topic, and there is a lack of evidence from large-scale studies conducted in China. This study aimed to investigate the potential associations between abortions, particularly repeated abortions, and the mental health status of postmenopausal women in Southwest China.
The data were obtained from the baseline survey of a multi-center natural population cohort study in cooperated with medical consortia in Southwest China. A standard structured questionnaire was used to assess abortion status among women of childbearing age. The 7-item Generalized Anxiety Disorder Scale (GAD-7) and the Patient Health Questionnaire-9 (PHQ-9) were used to evaluate psychological well-being. Subsequently, multiple logistic regression analysis was employed to examine the associations between the quantity and reasons for abortions and the mental health status of postmenopausal women.
A total of 9991 postmenopausal women were enrolled (mean age: 60.51 years), of whom 11.09% (1108 individuals) reported mental health problems (5.54% for depression and 8.27% for anxiety). Multiple logistic regression analysis revealed that, compared with women without any history of abortion, postmenopausal women who reported three or more abortions during their childbearing years were likely to have worse mental health conditions (OR [95% CI]: 1.37 [1.13, 1.67]). Additionally, women who reported a history of abortions for socio-economic reasons were also correlated with an increased risk of mental health issues after menopause (OR [95% CI]: 1.34 [1.08, 1.66]).
Women who reported a history of three or more abortions were at an increased risk of experiencing mental health issues after menopause. Reproductive-age women should enhance their contraceptive awareness to prevent unintended pregnancies and subsequent abortions. Healthcare institutions are recommended to strengthen psychological counseling for women who have undergone abortions.
Peer Review reports
Mental disorders are the leading cause of years lived with disability (YLD) globally [1], and people with severe mental health conditions tend to have a lifespan that is 10–20 years shorter than that of the general population [2]. Notably, females are more significantly affected by mental disorders than males [3]. According to a World Mental Health report, anxiety and depression, which account for approximately 59.9% of mental disorders worldwide, are the two most common mental health problems in females [1]. The age trend in their prevalence shows that the rate increases with age, peaks in the 50–69 age group, and then declines. This peak period includes a large proportion of postmenopausal women [1]. Data from the China Women’s Federation have indicated that women’s mental health issues remain prominent, yet their health needs are insufficiently addressed, particularly for postmenopausal women entering old age [4, 5]. Research has suggested that there is a greater likelihood of increased symptoms of depression or anxiety in women during postmenopause compared to their premenopausal years [6]. Data from the China Mental Health Survey have also revealed that anxiety and depression are no less common among older people than among the younger [7]. Therefore, the mental health issues of postmenopausal women should not be overlooked. It is crucial to thoroughly explore the risk factors affecting their mental health and implement targeted, effective preventive measures to improve their mental health status.
Research has indicated that adverse early life events are associated with poorer mental health outcomes later in life [4, 8]. In most cases, abortion is a stressful life event arising from an unwanted or unintended pregnancy and often poses challenges to women’s mental health [9]. A recent study has revealed that approximately one-quarter of women seeking a first-trimester abortion in China experience high perceived stress and probable depression [10]. Evidence from an prospective cohort study also indicated that abortion has an independent effect on mental health [11]. Regarding the persistence of adverse effects, studies from Germany and Korea have suggested that abortions during childbearing years are associated with long-term mental health problems, which can persist for up to ten years or even into menopause [12, 13]. However, current researches primarily focus on premenopausal women, and there is a lack of evidence regarding the association between abortion and mental health in postmenopausal women (see Supplementary Table 1). Additionally, there are also conflicting findings regarding the relationship between abortion and mental health [14,15,16,17]. Considering the impact of methodological heterogeneity between studies and the differences in abortion management policies across countries [18, 19], it appears crucial to gather additional data from diverse countries to gain a deeper understanding of these intricate associations.
Therefore, we aimed to explore whether abortions, particularly repeated abortions, experienced during reproductive years, are associated with a higher risk of mental health issues after menopause from the aspect of number and reasons of abortions, using cross-sectional data from a large cohort study conducted in Southwest China. The findings will provide theoretical references for contraception and women’s mental health care.
We conducted a cross-sectional study, using data obtained from the baseline survey of a natural population cohort study conducted by West China Hospital [20], with approval from the ethical community of West China Hospital, Sichuan University [No. (2020)145]. Residents older than 20 years from communities in Sichuan Province were invited to participate in this cohort, and all participants signed informed consent forms. To date, the cohort has completed the baseline survey in the cities of Chengdu, Ganzi, and Mianzhu from 2019 to 2021.
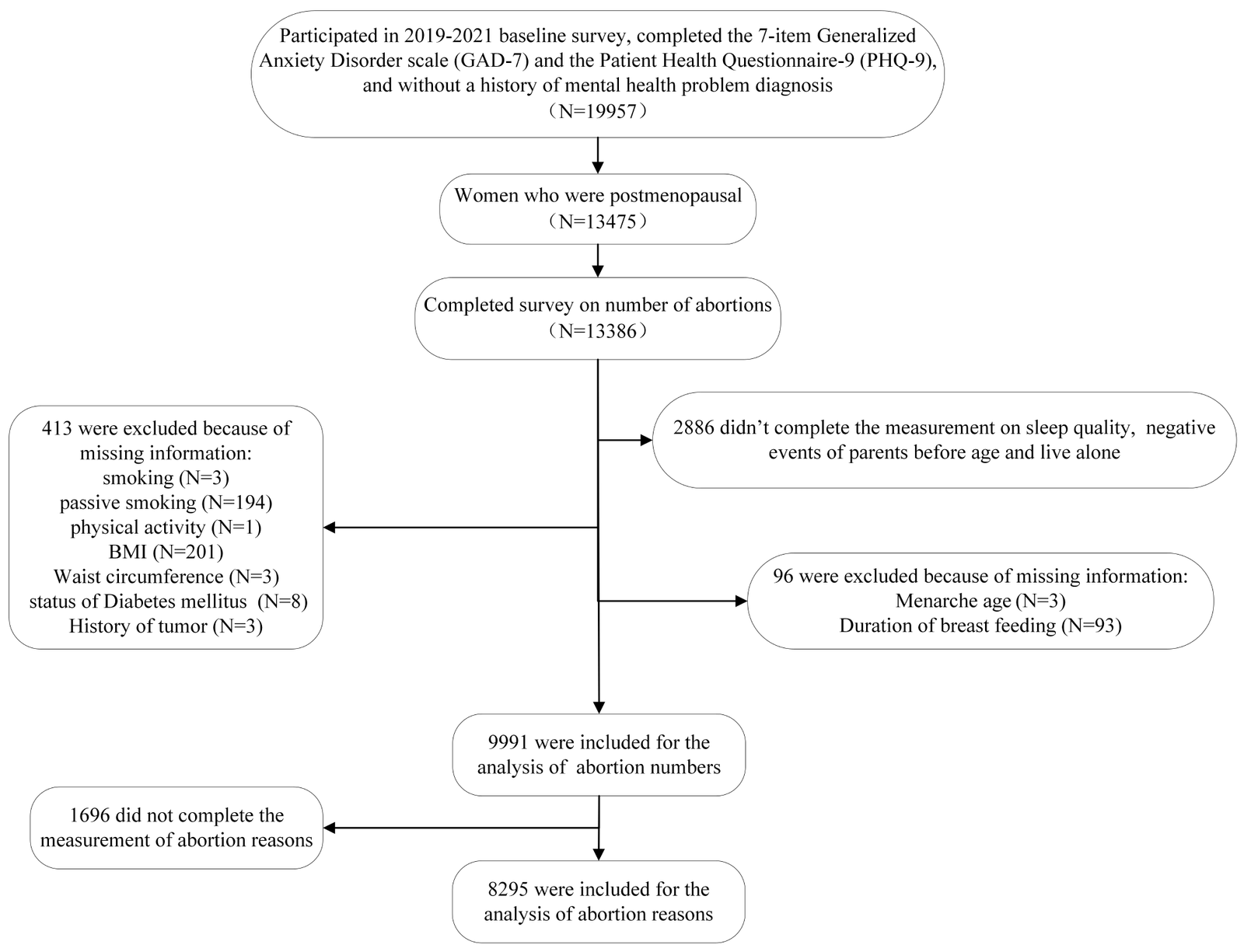
This cross-sectional study included baseline participants who were postmenopausal women, with no previous diagnosis of anxiety or depression by a doctor, and who had completed the current assessment for abortions and mental health status (depression and anxiety). Individuals who lacked information on some key covariates (such as behavioral lifestyle, and female reproductive history) were excluded (Fig. 1).
Abortion status during childbearing age was measured using a standard structured questionnaire, which included questions about abortion history during childbearing age, the number of abortions, and the primary reason for abortion. The reasons for abortion were categorized into three types: unhealthy pregnancy, planned parenthood, and other socioeconomic reasons such as economic conditions and personal preferences. Unhealthy pregnancy-related abortions referred to those caused by medical conditions resulting in either spontaneous or induced abortions. Planned parenthood-related abortions referred to those occurring under the context of the one-child policy (from 1979 to 2015, China implemented a nationwide family planning policy to mitigate the impact of immense population pressure on socioeconomic development, limiting each family to only one child) [21, 22]. Socioeconomic reasons-related abortions indicated abortions due to socioeconomic factors such as poor household income, unfavorable working conditions, high work stress, or overcrowded living conditions [23], which may result in women being unable or unwilling to have children.
In this study, we used the 7-item Generalized Anxiety Disorder Scale (GAD-7) to evaluate anxiety status [24], with total scores ≥ 5 as the cutoff point for the diagnosis of minor anxiety [25]. The Chinese version of this scale has been used for years, and its validity and reliability are well documented [26,27,28]. The Patient Health Questionnaire-9 (PHQ-9) was used to measure depression status [29], with total scores ≥ 5 as the cutoff point for the diagnosis of minor depression [25]. And the validity and reliability of its Chinese version are also satisfying [30, 31]. We had well-trained health professionals to assist in the whole survey. Women with scores indicating that they had mild or greater depression or anxiety, or both, were herein defined as having mental health problems [16, 32].
Covariates including age, marital status, education level, smoking and passive smoking status, drinking status, leisure-time physical activity (LTPA), menarche age, age at first birth, history of pregnancy-related diseases, number of births, duration of breastfeeding, menopause age, and history of diabetes, hypertension, and tumor were collected by self-report questionnaires. As introduced in a previous article, at least 11.25 MET-hours/week was regarded as reaching the WHO recommendation for the LTPA level [33]. The childbearing period was calculated by subtracting the menarche age from the menopause age.
Fasting blood samples were collected for routine biochemical analysis to assess health status, such as diabetes. The hypertension status and body mass index (BMI) were evaluated by objective measurements. BMI was defined as weight in kilograms divided by height squared in meters, with a BMI ≥ 24 indicating overweight [33]. Sleep quality was assessed using the Pittsburgh Sleep Quality Index (PSQI) [34]. The validity and reliability of its Chinese version are well documented [35, 36]. Participants were categorized into two groups based on their PSQI scores: good/perfect (0–10) and ordinary/poor (11–21) sleep.
Descriptive statistics were employed to outline the characteristics of the study participants. Continuous variables are reported as the mean and standard deviation (SD), while categorical variables are presented as frequencies (composition ratio). T-tests, chi-square tests, and Wilcoxon signed-rank tests were used to compare the baseline characteristics in women with and without mental health problems. Variables with a p-value < 0.1 in univariate analysis were selected for the construction of multiple logistic regression models (enter method). The correlation between the number and reasons for abortions and postmenopausal mental health status was first examined by the univariate logistic regression model, and then by the multiple logistic regression model after adjusting for potentially confounding variables. Comparisons of the number of abortions in women with different abortion reasons were performed using the chi-square test.
Given previous research findings that age, sleep quality, physical activity level, age at menopause, duration of breastfeeding, and number of live births are associated with women’s mental health [37,38,39,40,41,42], we conducted exploratory subgroup analyses. These analyses aimed to investigate whether the association between abortions during reproductive age and postmenopausal mental health varied across different subgroups. Moreover, for women who had experienced three or more abortions, univariate analysis was conducted to explore the differences in demographic characteristics and living behaviors between those with and without mental health problems.
All analyses were performed using R 4.1.2 software, with statistical significance set at p < 0.05.
Among 9991 postmenopausal women, 61.96% (6190 participants) of women reported at least one abortion during their childbearing age, among whom 13.07% (1306 participants) reported three or more abortions. A total of 11.09% (1108) of women reported mental health problems, with a prevalence of 5.54% (554 participants) for depression and 8.27% (826 participants) for anxiety. The mean ages were 60.67 years and 60.49 years for women with and without mental health problems, respectively. Women who reported mental health problems seemed to have a higher proportion of three or more previous abortions (16.61% vs. 12.63%, P < 0.05), and the proportion of abortions due to socio-economic reasons was higher in women with mental health problems than in those without (17.39% vs. 12.62%, P < 0.05). In addition, there were significant differences in the education level, status of smoking and passive smoking, negative events of parents before age 17, living alone, sleep quality, LTPA level, hypertension, history of tumor, age at first birth, duration of breastfeeding, history of pregnancy-related diseases, and number of births between the women with and without mental health problems (Table 1).
Study flow chart
Multiple logistic regressions showed that postmenopausal women who reported a history of three or more abortions during childbearing age were associated with worse mental health status than those without a history of abortion (OR [95% CI]: 1.37 [1.13, 1.67], Table 2). As for the leading reason for abortion, no association was found between policy-related abortion and postmenopausal mental health (OR [95% CI]: 0.96 [0.81, 1.14]) compared to women who had not reported an abortion. However, women who reported abortions due to socio-economic reasons were related with a higher risk of postmenopausal mental health problems (OR [95% CI]: 1.34 [1.08, 1.66]). Notably, women who reported abortions mainly due to planned parenthood exhibited a higher frequency of abortions in comparison to those mainly due to socio-economic reasons or health-related concerns (P < 0.001, Table 3).
Moreover, there appears to be a more notable association between abortion and anxiety than depression (Table 2). As for the number of abortions, although not statistically significant, we observed that an increased number of abortions seemed to be associated with a higher prevalence of depression (P for trend = 0.062). However, reporting for three or more abortions during reproductive age was significantly associated with postmenopausal anxiety symptoms (OR [95% CI]: 1.40 [1.12, 1.75]). In terms of the main causes of abortions, those due to other socioeconomic reasons were associated with both postmenopausal anxiety and depression symptoms (ORanxiety[95% CI]: 1.32 [1.04, 1.68], ORdepression[95% CI]: 1.36 [1.02, 1.81]). Additionally, abortions resulting from unhealthy pregnancy were also associated with postmenopausal anxiety symptoms (OR [95% CI]: 1.74 [1.16, 2.56]).
Although no statistically significant differences were observed in the relationship between abortion and mental health within each subgroup when stratified by age, sleep quality, LTPA level, age at menopause, duration of breastfeeding, and number of births (all P for interaction > 0.05), we did find a less pronounced association between abortion and mental health in women aged 65 years or younger, those with ordinary or poor sleep quality, those who breastfed for more than 12 months, and those with an age at menopause of 45 years or younger (all P>0.05, Fig. 2).
Subgroup analysis. uOR, unadjusted OR; aOR, adjusted OR; all models were adjusted for education level, smoking, passive smoking, hypertension, history of tumor, negative events of parents before 17 years old, living alone, age at first birth, history of pregnancy-related diseases, and (where appropriate) age, sleep quality, leisure-time physical activity, duration of breastfeeding, number of births, and age at menopause
Among women who reported three or more abortion experiences (see Supplementary Table 2), it appeared that those who actively engaged in physical activity had a lower likelihood of experiencing postmenopausal mental health issues, whereas those with poor sleep quality were more likely to encounter mental health problems (P < 0.05).
This study is the first to evaluate the real-world mental health status of postmenopausal women in Southwest China, and we found that repeated abortions, especially three or more, were associated with worse mental health conditions in postmenopausal women who had no prior history of anxiety or depression. Additionally, it seemed that abortions due to socio-economic reasons rather than planned parenthood were correlated with an increased risk of mental health problems after menopause compared to those who had not reported abortion.
In our study, approximately 11.09% of postmenopausal women in Southwest China reported mental health problems, with a prevalence of 5.54% for depression and 8.27% for anxiety. Similar to our findings, data from the China Mental Health Survey also revealed that anxiety was the most common mental health problem for Chinese female adults, followed by depression [7]. This study demonstrated that repeated abortions were positively related to postmenopausal mental health problems. One hypothesis is that repeated abortions may subject individuals to experience stress and negative emotions repeatedly, thus potentially increasing the risk of long-term anxiety and depression through the mechanism of rumination [43, 44]. It has been reported that rumination, characterized by repetitive negative thinking, could contribute to the development and persistence of psychopathology [45, 46]. Additionally, from the perspective of traditional Chinese medicine, recurrent abortions can lead to deficiencies in Qi and blood [47, 48], which may contribute to the development of anxiety and depression [49, 50]. We observed that recurrent abortions seemed to be more strongly associated with postmenopausal anxiety than depression, which could be related to the higher prevalence of anxiety among postmenopausal women in our study. Considering that women in this study may not have been fully forthcoming about their abortion histories [51], our findings are likely to underestimate the true mental health effects associated with abortion during the postmenopausal period.
Actually, the association between abortion and mental health is a debated topic. Studies that indicated negative findings often had limited sample sizes, failed to investigate the impact of repeated abortions on mental health, and paid less attention to whether abortion increased the risk of mental health issues in postmenopausal women (see Supplementary Table 1). Nevertheless, according to our findings in China, it is recommended that government or healthcare institutions improve contraceptive awareness among women of reproductive age through health education and provide proper contraceptive guidance to prevent unintended pregnancies and subsequent recurrent abortions. For women who have experienced abortions, attention should be given to enhancing psychological counseling and focusing on Qi and blood supplementation to improve their mental health.
To our knowledge, no prior study has examined the association between reasons for abortion and mental health in China. Our study found that women who reported abortions mainly due to planned parenthood (One-Child policy) had a significantly higher frequency of abortions than those due to socio-economic reasons or illness. However, it was abortions associated with socio-economic reasons, rather than those tied to planned parenthood, that showed an increased risk of postmenopausal mental health issues. It was reported that these women, who are now in the menopausal stage, were situated in a comparatively less developed socioeconomic environment during their reproductive years [52]. Those who reported abortions due to socio-economic reasons often suffered significant financial or work pressure at the time, unlike those who were willing to get pregnant but had abortions due to planned parenthood or medical concerns [53]. Studies have suggested that socioeconomic disadvantage, such as living in poverty and working under pressure, is an important driver of mental illness [54,55,56]. We assume that the relationship between abortion and mental health may significantly differ based on the reason for abortion (i.e., economic status), and this hypothesis needs further investigation. Nevertheless, based on what we have found so far, China should actively take measures to reduce socioeconomic-related abortions. For example [53]: (1) increasing financial support related to the reproductive conditions, (2) ensuring effective alignment between fertility policies and related public service systems, (3) establishing and improving childcare institutions and child welfare measures, and (4) providing more care for female employees, such as appropriately extending paid maternity leave and offering adequate paternity leave for men, to alleviate women’s reproductive anxiety and burden.
Our further subgroup analysis revealed a lack of correlation between abortion and mental health in women with ordinary/poor sleep quality, and women who experienced menopause at or before 45 years of age. Insomnia or poor sleep quality often persisted, and individuals dissatisfied with sleep quality currently were likely to experience poor sleep in the past [57]. Since women with poor sleep quality or who experienced menopause at or before 45 years of age were known to have subfecundity or less suitable time for pregnancy [58,59,60], the association between abortion and the risk of mental health problems may be masked. It was reported that breastfeeding was a protective factor for mental health. Our study observed that among women who breastfed for more than 12 months, the number of abortions was not statistically significantly associated with postmenopausal mental health. Further research is needed to determine whether breastfeeding can mitigate the negative mental health effects of repeated abortions. The association between abortions and mental health seemed to be more pronounced in women aged ≤ 65. Firstly, we supposed that the negative effects would gradually heal over time. Secondly, emotional fluctuations due to hormonal changes post-menopause may persist until age 65 [61], making their emotions potentially more susceptible to being influenced compared to those over 65. Moreover, we found that women who reported multiple abortions but did not have mental health problems were more likely to be physically active and have better sleep quality, which provides potential directions for preventing postmenopausal mental health problems in women who have undergone repeated abortions.
There were several limitations in this study. First, the data for this study were sourced from a cross-sectional survey, and information regarding abortion during the reproductive years was based on self-reports from the study participants, which may be affected by intentional underreporting or recall bias. However, there was a clear chronological order between abortion during childbearing age and postmenopausal mental health, which can help better identify the causality between them. Second, we did not specifically investigate the type of abortion (spontaneous or induced) or women’s values and preferences regarding abortion [62], and we could not further explore their differing effects on mental health, which requires additional research. Third, we did not collect information on the income levels, social support, or menopausal transition-related issues of these women, which may have influenced the results to some extent. Fourth, some studies have shown that abortion is associated with an increased risk of sleep disorders within the following 180 days [63], suggesting that these effects may not be independent. However, due to the current lack of high-quality research evidence establishing the association between abortion and long-term sleep quality, including during the postmenopausal period, we still included the current sleep quality as a covariate in the model alongside abortion. Fifth, we investigated only the primary reason for abortions, thus it was not possible to obtain a very precise estimate of the association between the causes of abortions and postmenopausal mental health. Despite the aforementioned limitations, this study utilized real-world data with a large sample size to establish a positive association between repeated abortions and long-term mental health status. In particular, this study highlighted the significant association of socioeconomic-related abortions with worse postmenopausal mental health conditions. Our findings will provide supportive evidence for women’s healthcare and contraception promotion efforts.
This study indicated that women who reported a history of three or more abortions were more likely to experience mental health problems after menopause. It is recommended that government or healthcare institutions improve contraceptive awareness among women of reproductive age through health education to prevent unintended pregnancies and resulting abortions. Additionally, enhancing relevant policies and economic support to reduce abortions due to socio-economic reasons is essential. Psychological counseling for women who have undergone abortions should also be strengthened. Further prospective studies are needed to elucidate the relationship between repeated abortions and postmenopausal mental health.
The datasets used in this study are available from the corresponding author on reasonable request.
The 7-item Generalized Anxiety Disorder Scale
The Patient Health Questionnaire-9
The Pittsburgh Sleep Quality Index
Leisure-time physical activity
Body mass index
Metabolic equivalents
world mental health report [https://iris.who.int/bitstream/handle/10665/356119/9789240049338-eng.pdf?sequence=1]
World Mental Health Report. The transition to mental health services for all [https://iris.who.int/bitstream/handle/10665/356121/9789240051904-chi.pdf?sequence=1]
Collaborators C-MD. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet (London England). 2021;398(10312):1700–12.
Article Google Scholar
Mental health of. the elderly [https://www.who.int/zh/news-room/fact-sheets/detail/mental-health-of-older-adults]
Women’s health. progress in key indicators and conceptual shifts [https://www.women.org.cn/art/2019/7/9/art_25_162249.html]
Mulhall S, Andel R, Anstey KJ. Variation in symptoms of depression and anxiety in midlife women by menopausal status. Maturitas. 2018;108:7–12.
Article PubMed Google Scholar
Huang Y, Wang Y, Wang H, Liu Z, Yu X, Yan J, Yu Y, Kou C, Xu X, Lu J, et al. Prevalence of mental disorders in China: a cross-sectional epidemiological study. Lancet Psychiatry. 2019;6(3):211–24.
Article PubMed Google Scholar
Richardson S, Carr E, Netuveli G, Sacker A. Adverse events over the life course and later-life wellbeing and depressive symptoms in older people. Int Psychogeriatr. 2023;35(5):243–57.
Article PubMed Google Scholar
Major B, Appelbaum M, Beckman L, Dutton MA, Russo NF, West C. Abortion and mental health: evaluating the evidence. Am Psychol. 2009;64(9):863–90.
Article PubMed Google Scholar
Zhang Q, Wang N, Hu Y, Creedy DK. Prevalence of stress and depression and associated factors among women seeking a first-trimester induced abortion in China: a cross-sectional study. Reproductive Health. 2022;19(1):64.
Article PubMed PubMed Central Google Scholar
Sullins DP. Affective and substance abuse disorders following abortion by Pregnancy Intention in the United States: a longitudinal cohort study. Med (Kaunas Lithuania). 2019;55(11).
Jacob L, Kostev K, Gerhard C, Kalder M. Relationship between induced abortion and the incidence of depression, anxiety disorder, adjustment disorder, and somatoform disorder in Germany. J Psychiatr Res. 2019;114:75–9.
Article PubMed Google Scholar
Jung SJ, Shin A, Kang D. Menarche age, menopause age and other reproductive factors in association with post-menopausal onset depression: results from Health examinees Study (HEXA). J Affect Disord. 2015;187:127–35.
Article PubMed Google Scholar
Biggs MA, Upadhyay UD, McCulloch CE, Foster DG. Women’s Mental Health and Well-being 5 years after receiving or being denied an abortion: a prospective, longitudinal cohort study. JAMA Psychiatry. 2017;74(2):169–78.
Article PubMed Google Scholar
Munk-Olsen T, Laursen TM, Pedersen CB, Lidegaard Ø, Mortensen PB. Induced first-trimester abortion and risk of mental disorder. N Engl J Med. 2011;364(4):332–9.
Article PubMed Google Scholar
van Ditzhuijzen J, Ten Have M, de Graaf R, van Nijnatten C, Vollebergh WAM. Long-term incidence and recurrence of common mental disorders after abortion. A Dutch prospective cohort study. J Psychiatr Res. 2018;102:132–5.
Article PubMed Google Scholar
The facts about. abortion and mental health [https://www.apa.org/monitor/2022/09/news-facts-abortion-mental-health#]
Global Abortion Policies Database. [https://abortion-policies.srhr.org/]
After Roe Fell. Abortion Laws by State [https://reproductiverights.org/maps/abortion-laws-by-state/]
Fan P, Zhang S, Wang W, Yang Z, Tan W, Li S, Zhu C, Hu D, Zhou X, Tian Z, et al. The design and implementation of natural population cohort study Biobank: a multiple-center project cooperation with medical consortia in Southwest China. Front Public Health. 2022;10:996169.
Article PubMed PubMed Central Google Scholar
China’s One Child Policy. [https://scholar.harvard.edu/files/martinwhyte/files/chinas_one_child_policy.pdf]
Birth policy transition in China. [https://news.cgtn.com/news/2021-06-03/Birth-policy-transition-in-China-10NjYlhrfEY/index.html]
Socioeconomic Factors. [https://www.cdc.gov/dhdsp/health_equity/socioeconomic.htm]
Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–7.
Article PubMed Google Scholar
Stocker R, Tran T, Hammarberg K, Nguyen H, Rowe H, Fisher J. Patient Health Questionnaire 9 (PHQ-9) and general anxiety disorder 7 (GAD-7) data contributed by 13,829 respondents to a national survey about COVID-19 restrictions in Australia. Psychiatry Res. 2021;298:113792.
Article PubMed PubMed Central Google Scholar
He XY, Li CB, Qian J, Cui HS, Wu WY. Reliability and validity of a generalized anxiety disorder scale in general hospital outpatients. Shanghai Arch Psychiatry. 2010;22(4):200–3.
Zeng QZ, He YL, Liu H, Liao JM, Chen JX, Xu HN, Wang JY. Reliability and validity of Chinese version of the Generalized Anxiety Disorder 7-item(GAD-7) scale in screening anxiety disorders in outpatients from traditional Chinese internal department. Chin Mental Health J. 2013;27(3):163–168.
Qu S, Sheng L. Diagnostic test of screening generalized anxiety disorders in general hospital psychological department with GAD-7. Chin Mental Health J. 2015;29(12):939–944.
Levis B, Benedetti A, Thombs BD. Accuracy of Patient Health Questionnaire-9 (PHQ-9) for screening to detect major depression: individual participant data meta-analysis. BMJ (Clinical Res ed). 2019;365:l1476.
Google Scholar
Chen S, Chiu H, Xu B, Ma Y, Jin T, Wu M, Conwell Y. Reliability and validity of the PHQ-9 for screening late-life depression in Chinese primary care. Int J Geriatr Psychiatry. 2010;25(11):1127–33.
Article PubMed Google Scholar
Sun XY, Li YX, Yu CQ, Li LM. Reliability and validity of depression scales of Chinese version: A systematic review. Chin J Epidemiol. 2017;38(1):110–116.
Coleman PK. Abortion and mental health: quantitative synthesis and analysis of research published 1995–2009. Br J Psychiatry: J Mental Sci. 2011;199(3):180–6.
Article Google Scholar
Chen H, Zhang R, Zheng Q, Yan X, Wu S, Chen Y. Impact of body mass index on long-term blood pressure variability: a cross-sectional study in a cohort of Chinese adults. BMC Public Health. 2018;18(1):1193.
Article PubMed PubMed Central Google Scholar
Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213.
Liu XCH, Tang MQ, Hu L, Wang AZ, Wu HX, Zhao GF, Gao CN, % LWS. Reliability and validity of the Pittsburgh sleep quality index. Chin J Psychiatry. 1996;29(2):103–7.
Google Scholar
Taoying L, Yan L, Ping X, Guangqing Z, Darong WJCM. Analysis on reliability and validity of the Pittsburgh sleep quality index. 2014.
Georgakis MK, Thomopoulos TP, Diamantaras AA, Kalogirou EI, Skalkidou A, Daskalopoulou SS, Petridou ET. Association of Age at Menopause and Duration of Reproductive Period with Depression after Menopause: a systematic review and Meta-analysis. JAMA Psychiatry. 2016;73(2):139–49.
Article PubMed Google Scholar
Tsunoda K, Matsumura K, Inano H, Hatakeyama T, Tsuchida A, Inadera H. Association of infants’ feeding pattern up to 2 years postpartum with mothers’ mental and physical health: the Japan Environment and Children’s study. J Affect Disord. 2023;327:262–9.
Article PubMed Google Scholar
Wang H, Chen M, Xin T, Tang K. Number of children and the prevalence of later-life major depression and insomnia in women and men: findings from a cross-sectional study of 0.5 million Chinese adults. BMC Psychiatry. 2020;20(1):267.
Article PubMed PubMed Central Google Scholar
Mental, Health. and Aging [https://www.cdc.gov/aging/olderadultsandhealthyaging/mental-health-and-aging.html]
Pearce M, Garcia L, Abbas A, Strain T, Schuch FB, Golubic R, Kelly P, Khan S, Utukuri M, Laird Y, et al. Association between Physical Activity and Risk of Depression: a systematic review and Meta-analysis. JAMA Psychiatry. 2022;79(6):550–9.
Article PubMed PubMed Central Google Scholar
Scott AJ, Webb TL, Martyn-St James M, Rowse G, Weich S. Improving sleep quality leads to better mental health: a meta-analysis of randomised controlled trials. Sleep Med Rev. 2021;60:101556.
Article PubMed PubMed Central Google Scholar
Michl LC, McLaughlin KA, Shepherd K, Nolen-Hoeksema S. Rumination as a mechanism linking stressful life events to symptoms of depression and anxiety: longitudinal evidence in early adolescents and adults. J Abnorm Psychol. 2013;122(2):339–52.
Article PubMed PubMed Central Google Scholar
Baumeister RF, Gailliot M, DeWall CN, Oaten M. Self-regulation and personality: how interventions increase regulatory success, and how depletion moderates the effects of traits on behavior. J Pers. 2006;74(6):1773–801.
Article PubMed Google Scholar
Ehring T. Thinking too much: rumination and psychopathology. World Psychiatry: Official J World Psychiatric Association (WPA). 2021;20(3):441–2.
Article Google Scholar
Rumination A. Cycle of Negative Thinking [https://www.psychiatry.org/News-room/APA-Blogs/Rumination-A-Cycle-of-Negative-Thinking]
Can abortion cause. Qi deficiency [https://m.baidu.com/bh/m/detail/ar_15294976938398764910]
How to recuperate. Qi and blood after abortion [https://m.baidu.com/bh/m/detail/ar_2872123000335918039]
Lai YD, Jin HB. The association between blood deficiency, liver depression and depression. Sichuan J Traditional Chin Med. 2009;27(2):30–1.
Google Scholar
Luo H, Li LR, Wang Q. Correlation between qi deficiency constitution and disease: a bibliometric analysis of 332 observational studies. Tianjin J Traditional Chin Med. 2019;36(7):625–30.
Google Scholar
Yan T, Tourangeau R. Detecting underreporters of abortions and miscarriages in the national study of family growth, 2011–2015. PLoS ONE. 2022;17(8):e0271288.
Article PubMed PubMed Central Google Scholar
Statistics Bureau. Great changes in China’s economic and social development since 1978 [https://www.gov.cn/jrzg/2013-11/06/content_2522445.htm]
Zhang W-Z, Zheng J-Y. The willingness of women of childbearing age to have a second child in Lanzhou under the universal two-child policy. Child Youth Serv Rev. 2021;121:105732.
Article Google Scholar
Ridley M, Rao G, Schilbach F, Patel V. Poverty, depression, and anxiety: Causal evidence and mechanisms. Science (New York, NY). 2020;370(6522).
Kivimäki M, Batty GD, Pentti J, Shipley MJ, Sipilä PN, Nyberg ST, Suominen SB, Oksanen T, Stenholm S, Virtanen M, et al. Association between socioeconomic status and the development of mental and physical health conditions in adulthood: a multi-cohort study. Lancet Public Health. 2020;5(3):e140–9.
Article PubMed Google Scholar
Rugulies R, Aust B, Greiner BA, Arensman E, Kawakami N, LaMontagne AD, Madsen IEH. Work-related causes of mental health conditions and interventions for their improvement in workplaces. Lancet (London England). 2023;402(10410):1368–81.
Article PubMed Google Scholar
Association CSR. Guidelines for diagnosis and treatment of insomnia in China. Natl Med J China. 2017;97(24):1844–56.
Google Scholar
Hyland A, Piazza K, Hovey KM, Tindle HA, Manson JE, Messina C, Rivard C, Smith D, Wactawski-Wende J. Associations between lifetime tobacco exposure with infertility and age at natural menopause: the women’s Health Initiative Observational Study. Tob Control. 2016;25(6):706–14.
Article PubMed Google Scholar
Kloss JD, Perlis ML, Zamzow JA, Culnan EJ, Gracia CR. Sleep, sleep disturbance, and fertility in women. Sleep Med Rev. 2015;22:78–87.
Article PubMed Google Scholar
Breast-feeding and. Fertility regulation: current knowledge and programme policy implications. Bull World Health Organ. 1983;61(3):371–82.
Google Scholar
Menopause Subgroup CSoOaG, Chinese Medical Association. [The 2023 Chinese menopause symptom management and menopausal hormone therapy guidelines]. Zhonghua Fu Chan Ke Za Zhi. 2023;58(1):4–21.
Google Scholar
Reardon DC, Rafferty KA, Longbons T. The effects of abortion decision rightness and decision type on women’s satisfaction and Mental Health. Cureus. 2023;15(5):e38882.
PubMed PubMed Central Google Scholar
Reardon DC, Coleman PK. Relative treatment rates for sleep disorders and sleep disturbances following abortion and childbirth: a prospective record-based study. Sleep. 2006;29(1):105–6.
Article PubMed Google Scholar
Download references
We would like to thank all participants of this study.
This work was supported by the Scientific and Technological Innovation 2030 – Major Project (2023ZD0505300, 2023ZD0505304). The funder had no role in the study design, data collection, analysis, data interpretation or manuscript preparation.
Department of Clinical Research and Management, Center of Biostatistics, Design, Measurement and Evaluation (CBDME), West China Hospital, Sichuan University, Chengdu, Sichuan, 610041, P.R. China
Xu Li & Lin Li
Department of Neurology, West China Hospital, Sichuan University, Chengdu, Sichuan, 610041, P.R. China
Anjiao Peng & Lei Chen
You can also search for this author in PubMed Google Scholar
You can also search for this author in PubMed Google Scholar
You can also search for this author in PubMed Google Scholar
You can also search for this author in PubMed Google Scholar
X.L. conceived the study, and contributed to the design, analysis, and manuscript preparation. AJ.P. supervised the work, and critically revised and reviewed the manuscript. L.L. contributed to the data analysis and results presentation. L.C. contributed to the conception and revised the final draft of the manuscript. All authors reviewed and approved the final manuscript.
Correspondence to Lei Chen.
This study was approved by the ethical community of West China Hospital, Sichuan University. We confirmed that all methods were performed in accordance with relevant guidelines and regulations to protect human subjects. All participants read and signed written informed consent forms.
Not applicable.
The authors declare no competing interests.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Below is the link to the electronic supplementary material.
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
Reprints and permissions
Li, X., Peng, A., Li, L. et al. The association between repeated abortions during childbearing age and the psychological well-being of postmenopausal women in Southwest China: an observational study. BMC Pregnancy Childbirth 24, 805 (2024). https://doi.org/10.1186/s12884-024-07005-w
Download citation
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12884-024-07005-w
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Advertisement
ISSN: 1471-2393
By using this website, you agree to our Terms and Conditions, Your US state privacy rights, Privacy statement and Cookies policy. Your privacy choices/Manage cookies we use in the preference centre.
© 2024 BioMed Central Ltd unless otherwise stated. Part of Springer Nature.